TMJ Surgery - The temporomandibular joint is a hinge-like joint placed where your jawbone and skull connect. The TMJ enables your jaw to slide up and down allowing you to talk, chew, etc.
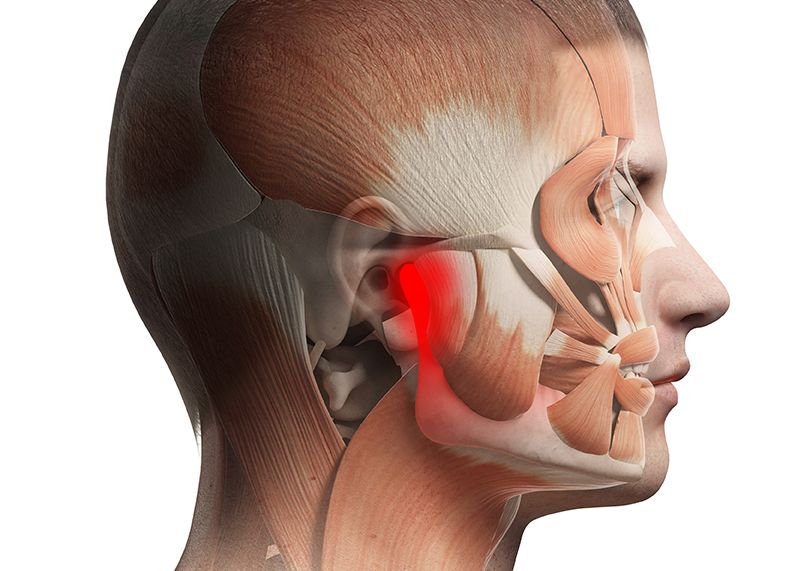
A TMJ disorder leads to ache, rigidity or lack of movement in your jaw joint, restricting you from using your jaw's range of movement.
What is TMJ Surgery?
Surgery is the option to treat a TMJ disorder if more conventional treatments, like oral splints or mouthguards, fail to reduce the severity of your symptoms. For some people, surgery may be required to make full use of their TMJ.
Oral and maxillofacial surgeon like Dr. Anurag Bhargava is a renowned surgeon to perform TMJ surgery.
The doctor may suggest TMJ surgery if:
- You can't open or close your mouth.
- On facing problems while eating or drinking because of jaw ache or immovability.
- You feel ongoing, acute pain or tenderness when you open or close your mouth.
- When even rest and other non-surgical treatments don't work.
- When specific diseases in your jaw have been diagnosed with MRI.
The doctor may not suggest TMJ surgery if:
- Your TMJ symptoms are not very serious. In case your jaw makes a clicking sound when you open it but if there is no pain related to it you may not need surgery.
- When the symptoms are not very consistent such as excessive talking, chewing a lot of hard food or continuous gum chewing that cause fatigue in your TMJ. In this case, your doctor may recommend you to rest your jaw for a few days.
- Even when you have some pain when you open or close your mouth the doctor may not suggest surgery because of the complications involved. They may recommend medication, physical therapy or lifestyle modification to lower the symptoms.
- It is necessary to be examined by a dentist or an oral surgeon expert in TMD. Oral and maxillofacial surgeon like Dr. Anurag Bhargava is the right doctor for consultation.
- They will do a careful study of your symptomatic history, clinical presentation, and radiological findings to ascertain if surgery will be required for your symptoms. When nonsurgical alternatives are unsuccessful, surgery is performed.
Types of TMJ Surgery
There are different types of TMJ surgery depending on your symptoms:
1. Arthroscopy
Arthroscopy procedure is performed by making a small hole or a few small holes in the skin above the joint.
A tube called a cannula is then inserted through the hole and into the joint. Then, your surgeon will insert an arthroscope into the cannula. The arthroscope is an instrument with a light and camera that's used to visualize your joint.
Then the surgeon operates on the joint using small surgical tools that are inserted through the cannula.
TMJ Arthroscopy has a faster recovery time. It also allows your doctor to do complex procedures on the joint like:
- medication injection
- scar tissue removal
- joint reshaping
- pain or swelling relief
2. Arthrocentesis
Arthrocentesis is performed by injecting fluid into your joint. The fluid washes out any chemical byproducts of inflammation and can help minimize the pressure that causes the joint to be rigid or painful. This can help you restore some of your jaw's range of motion.
This is a small procedure. You can return home on the same day. TMJ Arthrocentesis is often the first-line treatment as it is less invasive and has a high success rate in comparison to some of the other more risky procedures.
3. Open-joint Surgery
Open-joint surgery comprises opening a cut a few inches long over the joint so your doctor can operate on the joint itself.
This type of surgery is performed for a severe TMJ disorder that involves:
- The fusion of the joint tissue, cartilage or bone.
- Tissue or bone growth that stops the joint from moving.
- Inability to reach the TMJ joint with arthroscopy.
By performing open-joint surgery, your doctor will be able to take out bony growths or excess tissue. They also mend or reposition the disc if it's out of place or harmed.
If your disc is irreparable, a discectomy may be performed. Your surgeon may replace your disc with an artificial disc or your tissue.
When the bony structures of the joint are involved, the doctor may remove the diseased bone of the jaw joint.
Though open surgery has a higher recovery time than an arthroscopic procedure but has a higher success rate.
Oral and maxillofacial surgeon like Dr. Anurag Bhargava performs the above surgeries with expertise.
Recovery from TMJ Surgery
TMJ surgery recovery depends on the person and the type of surgery performed. In most of the TMJ surgeries, you will be able to go home the same day.
Take a few days off from your work to take time to rest. After the surgery, you may have a bandage around your head to secure the wound dressing.
- For a few days after the surgery follow the following precautions for quick recovery.
- Take nonsteroidal anti-inflammatory drugs for any pain if your doctor suggests it. In the case of kidney problems or bleeding disorders, such drugs should not be taken.
- Stick to a liquid diet and avoid solid foods. Drink a lot of water after surgery.
- To overcome swelling apply a cold compress.
- Make sure to cover up your bandage before bathing or showering.
- Regularly change bandage before bathing or showering. Whenever you change the bandages apply antibiotic creams or ointments.
- Heating pads or microwaving a damp cloth helps to apply heat after surgery.
- Wear a brace on your jaw till the doctor asks you to remove it.
- Patients may need to make lifestyle changes to avoid exacerbating TMJ disorder symptoms in the future. This may include avoiding certain foods, practicing stress-management techniques, and maintaining good posture.
- Patients will need to attend follow-up appointments with their TMJ surgeon to monitor healing and ensure that the surgery was successful.
See your doctor a few days after the surgery to receive further suggestions related to your TMJ.
If the stitches do not dissolve on their own, the doctor may need to remove the stitches. The doctor may recommend medications for pain or any infections.
A physical therapist may help you regain motion in your jaw which can be hindered by swelling.
Complications from TMJ Surgery
The obvious complication of TMJ surgery is a permanent loss in the range of motion.
Other complications are:
- The wound of facial nerves leading to a partial loss of facial muscle movement or loss sensation.
- Harm to nearby tissue such as blood vessels, the bottom of the skull or anatomy related to your hearing.
- During or after the surgery infections around the surgical site.
- Continuous pain or restricted range of motion.
- Frey syndrome that causes abnormal face sweating.
Is there a Reoccurrence of TMJ Pain?
TMJ pain can persist even after you've had surgery as debris can accumulate again in the joint or inflammation can occur again.
It can also return by grinding your teeth when you are in a panic or while you sleep.
TMJ pain can come back if you suffer from rheumatoid arthritis.
What to Consult from the Doctor?
Before you go for TMJ surgery, ask your doctor:
- If surgery isn't recommended for me, how can I relieve my pain or increase my range of motion?
- What is the intensity of my pain before I have surgery?
- Which type of surgery do you suggest for me? Why?
- Whether a physical therapist can help?
- Should I stop eating hard or chewing foods?
- Are there any risks involved if I decide not to have the surgery?
Recommendations for You
See your doctor if your jaw pain is perilous to your life or it prevents you from eating or drinking.
You may not require surgery if nonsurgical therapies, medicines or lifestyle changes relieve your TMJ pain. Surgery is recommended in severe cases.
Let your doctor know if more conventional treatments are not helpful or the symptoms are serious.
Oral and maxillofacial surgeon in Indore like Dr. Anurag Bhargava will provide a cure for your trouble.
Frequently Asked Questions (FAQ) Related to TMJ Surgery
1. How long does the recovery process take after TMJ surgery?
Recovery time after TMJ surgery varies depending on the type of procedure performed and the individual’s overall health. Typically, less invasive procedures like arthrocentesis or arthroscopy have a shorter recovery period, ranging from a few days to a couple of weeks. For more invasive surgeries, such as open-joint surgery, recovery might take several weeks to a few months. During recovery, it's essential to follow your surgeon’s instructions, including resting the jaw, sticking to a soft or liquid diet, and attending follow-up appointments for proper healing.
2. Will I be able to eat normally after surgery?
Immediately after TMJ surgery, you will likely need to stick to a liquid or soft food diet to avoid placing stress on your jaw. Gradually, as your jaw heals and gains strength, you’ll be able to transition back to solid foods, typically within a few weeks. Your surgeon will provide detailed dietary guidelines for each stage of recovery. Full resumption of normal eating habits will depend on the type of surgery and the pace of your healing.
3. Is TMJ surgery painful?
Pain levels vary depending on the type of TMJ surgery. Minimally invasive procedures like arthroscopy and arthrocentesis usually cause less discomfort and have a shorter recovery time. You will likely experience some level of discomfort or pain post-surgery, which can be managed with prescribed pain medications or over-the-counter anti-inflammatory drugs, as recommended by your doctor. Most patients report that the pain subsides within a few days to weeks. Your doctor may also suggest physical therapy or jaw exercises to help alleviate any post-operative discomfort.
4. How do I know if I am a candidate for surgery?
Not everyone with TMJ disorders needs surgery. Surgery is typically recommended only when non-surgical treatments (such as physical therapy, medication, or mouthguards) fail to relieve symptoms, or when the TMJ is severely damaged due to injury, arthritis, or other underlying conditions. If you experience chronic pain, difficulty opening or closing your jaw, or jaw immobility that interferes with daily life, you may be a candidate for surgery. A thorough evaluation by an oral and maxillofacial surgeon, including diagnostic imaging such as an MRI or CT scan, will determine if surgery is necessary for your condition.
5. What can I expect at my follow-up appointment?
Your follow-up appointment is crucial to monitor your recovery and ensure the surgery was successful. During the visit, your surgeon will evaluate the healing of your incision site and check the range of motion in your jaw. They may also remove stitches if necessary and provide guidance on when you can resume regular activities, including chewing and speaking normally. Depending on your recovery progress, they may recommend additional physical therapy or prescribe further medications to manage pain and swelling. Be sure to report any persistent pain or unusual symptoms during your follow-up visit.

