The most common form of internal TMJ dislocation is anterior misalignment or displacement of the articular disc above the condyle. Its symptoms include localized joint pain and popping on the jaw movement. History and physical examination help in the right diagnosis. Treatment involves analgesics, jaw rest, muscle relaxation, physical therapy, and bite splints. Surgery may be required in adverse cases by oral and maxillofacial surgeons like Dr. Anurag Bhargava.
TMJ Dislocation
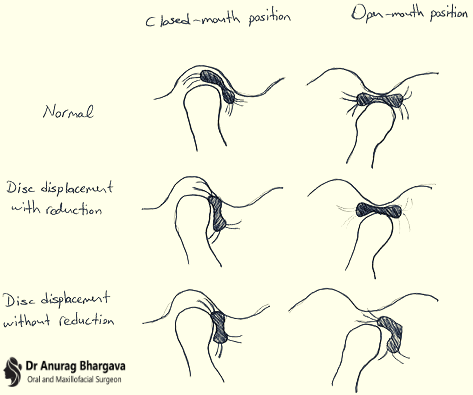
Abnormal jaw mechanics can be due to birth or acquired asymmetries or to the sequelae of trauma or arthritis. If the disc remains anterior, the displacement is said to be without reduction. It may result in restricted jaw opening and pain in the ear and around the temporomandibular joint. If at some point in the joint's excursion, the disc returns to the head of the condyle, the dislocation is termed to be with reduction.
Get to know about Temporomandibular Joint Disorders
Symptoms and Treatment of TMJ Disc Dislocation with Reduction
Disc displacement with reduction causes a painless clicking when the mouth is opened. While chewing hard foods one may experience pain.
The diagnosis of disc displacement with reduction needs observation of the jaw when the mouth is opened. When the jaw is opened > 10 mm a click is heard, as the disc pops back over the head of the condyle. The condyle stays on the disc during the further opening. Usually, another more reciprocal click is heard during closing when the condyle slips over to the posterior rim of the disc slips forward.
TMJ Disc dislocation with reduction does not require treatment if the patient can open jaw wide enough without discomfort. If pain persists, mild analgesics can be administered. Some patients benefit from doing slow jaw-motion exercises using commercially available mechanical tools.
If the duration is < 6 months, an anterior repositioning brace may be used to position the mandible forward and on the disc. A brace is a horseshoe-shaped appliance of tough, transparent plastic made to fit compactly over the teeth of one arch. Its chewing surface is made to hold the mandible forward when the patient closes on the brace. In this position, the disc is always on the head of the condyle. The brace is slowly adjusted to allow the mandible to move posteriorly. If the disc stays with the condyle as the superior head of the external pterygoid stretches, the disc is known to be captured. The longer the disc is displaced, the more distorted it becomes and little chance of repositioning to succeed.
Symptoms and Treatment of TMJ Disc Dislocation without Reduction
TMJ Disc dislocation without reduction with the limited opening is uncommon. It is seen that progression to chronic and disabling intracapsular TMJ disease is uncommon. It is often self-limiting or fluctuating over time. Women are more prone to disc displacement without reduction than men. It is more common in young and middle-aged women.
Sign of Disc Displacement without Reduction
- Restriction of movement to the normal joint.
- No intracapsular sounds identified unless chronic and associated with a change in bony surfaces.
- A maximum passive stretch is less than 40 mm including the vertical incisal overlap.
- Deflection of the mandible to the involved joint side on opening and protrusion.
Causes and Risk Factors of TMJ Disc Displacement
TMJ (Temporomandibular Joint) disc displacement can stem from various factors, ranging from inherent conditions to external influences. Understanding the causes and risk factors is crucial for better management and prevention. Let's delve into the intricacies:
1. Trauma:
- Cause: Direct impact or injury to the jaw can disrupt the delicate balance of the TMJ components.
- Risk Factor: Individuals involved in contact sports or those prone to accidents may be at a higher risk.
2. Arthritis:
- Cause: Inflammatory joint conditions like rheumatoid arthritis can affect the TMJ.
- Risk Factor: People with a history of arthritis or autoimmune disorders may have an increased susceptibility.
3. Congenital Factors:
- Cause: Structural abnormalities present at birth can contribute to TMJ issues.
- Risk Factor: Individuals with congenital jaw or joint anomalies may be predisposed to disc displacement.
4. Dental Occlusion Irregularities:
- Cause: Poor bite alignment or irregularities in dental occlusion can impact TMJ function.
- Risk Factor: Those with malocclusion or those who have undergone extensive dental work may be at risk.
5. Bruxism (Teeth Grinding):
- Cause: Persistent teeth grinding, often during sleep, can strain the TMJ.
- Risk Factor: Individuals with untreated bruxism are more likely to experience TMJ-related issues.
6. Stress and Anxiety:
- Cause: Emotional stress and anxiety can contribute to jaw clenching, affecting the TMJ.
- Risk Factor: Individuals with high-stress lifestyles may be prone to developing TMJ disorders.
7. Hormonal Influences:
- Cause: Hormonal fluctuations, particularly in women, can impact joint laxity.
- Risk Factor: Women, especially during puberty, pregnancy, or menopause, may experience increased vulnerability.
8. Poor Posture:
- Cause: Incorrect neck and head posture can strain the TMJ and surrounding muscles.
- Risk Factor: Individuals with occupations or habits leading to poor posture may face a higher risk.
Understanding these causes and risk factors empowers individuals to adopt preventive measures and seek timely intervention when necessary.
Symptoms Patients Often Face
These are precisely when the closed lock takes place and can relate it to a specific event.
- Pain is often localized to the preauricular area.
- Pain may be described as intense and is closely related to joint movement, particularly at the point limitation of movement.
- If inflammation develops, the pain may be constant and be accentuated by joint movement and joint loading.
- The patient displays worries regarding the sudden decline in mandibular movement as a result of the closed lock.
Also, learn about Temporomandibular Joint Ankylosis
Types of TMJ Disc Displacement
1. Disc Displacement with Reduction:
- Characteristics: Painless clicking during mouth opening, often accompanied by pain while chewing hard foods.
- Diagnosis: Audible click when the mouth opens > 10 mm, with the disc popping back over the condyle.
2. Disc Displacement without Reduction:
- Characteristics: Limited jaw opening, pain in the ear and around the joint, and possible deflection of the mandible to the affected side.
- Diagnosis: No significant click during mouth opening, with the disc remaining anterior and restricted jaw movement.
3. Chronic Cases:
- Characteristics: Elongation of ligaments, altered disc morphology, and potential impact on adjacent structures.
- Diagnosis: Magnetic resonance imaging (MRI) is crucial for confirming chronic disc displacement.
4. Acute Cases:
- Characteristics: Sudden onset of symptoms like a closed lock, requiring prompt intervention.
- Treatment: Manual manipulation, anterior positioning appliances, and stabilization appliances may be considered.
Understanding the nuances of these types of disc displacement aids both patients and healthcare professionals in navigating treatment options effectively.
Investigation
- Obtain a thorough medical history, including details related to pain and dysfunction.
- Performed on head, neck, and teeth to rule out local pathology or other sources of pain and to assess joint function.
- The downward force applied to the mandibular incisors produces a minimal increase in the range of opening.
- Difficulty in mouth opening as a result of muscle disorders is usually variable in terms of the range of opening.
- Loading of the involved joint is painful.
- Confirm the diagnosis on a magnetic resonance imaging (MRI) scan of the TMJ.
- Determine whether the disc displacement without reduction with the limited opening is chronic.
- The clinical diagnosis becomes less clear if disc displacement is chronic, as the ligaments become further elongated and the morphology of the disc becomes changed.
Diagnosis of TMJ Disc Dislocation without Reduction
A diagnosis of disc displacement without reduction with the limited opening can be made upon patient history, clinical examination, and related tests.
Treatment of TMJ Disc Dislocation without Reduction
Approaches to acute cases may be different from chronic cases.
A common treatment for acute cases:
When a patient experiences a closed lock for 1 week or less then we refer him to an oral medicine specialist or oral and maxillofacial surgeon in Indore.
Consider attempting manual manipulation to regain the normal discondyle relationship. Then the patient could wear an anterior positioning appliance for the first few days followed by nighttime use only. Once stability has come, a stabilization appliance may be considered for nighttime use.
In serious cases, a minimally invasive surgical procedure arthroscopy could be considered to return the disc to a normal functional relationship with the condyle.
Treatment of Chronic Cases
In chronic cases, the oral and maxillofacial surgeon in Indore will explore surgical approaches.
For controlling the pain, involve a physical therapist to assist with pain control and regaining range of opening.
Prevention Tips for TMJ Disc Dislocation
Preventing TMJ (Temporomandibular Joint) disc dislocation involves adopting habits and practices that promote jaw health and reduce stress on the joint. Here are practical tips to safeguard against this condition:
1. Maintain Good Posture
Be conscious of your head and neck posture. Sit and stand with your shoulders back, and avoid cradling the phone between your shoulder and ear.
2. Manage Stress
Incorporate stress management techniques into your routine, such as deep breathing, meditation, or yoga. Stress reduction can alleviate jaw-clenching tendencies.
3. Avoid Excessive Jaw Movement
Limit activities that involve prolonged or extreme jaw movements, such as wide yawning or gum chewing. These actions can strain the TMJ.
4. Practice Relaxation Exercises
Integrate jaw relaxation exercises into your daily routine. Gently massage the jaw muscles and perform simple jaw stretches to release tension.
5. Be Mindful of Teeth Grinding (Bruxism)
If you grind your teeth, especially during sleep, consider wearing a nightguard. This protective dental device helps minimize the impact of teeth grinding on the TMJ.
6. Maintain Dental Health
Attend regular dental check-ups to address any dental issues promptly. Proper dental care can prevent complications that may contribute to TMJ problems.
7. Stay Hydrated
Dehydration can affect muscle function, including those around the jaw. Ensure adequate water intake to support overall muscle health.
8. Avoid Excessive Chewing
Minimize the consumption of hard or tough foods that require excessive chewing. Opt for softer, more easily chewable options to reduce strain on the jaw.
9. Use Proper Pillow Support
Choose a supportive pillow that maintains proper head and neck alignment during sleep. This can contribute to overall spinal health and reduce strain on the TMJ.
10. Regular Jaw Exercises
Incorporate gentle jaw exercises into your daily routine. Consult with a healthcare professional for guidance on exercises that promote jaw flexibility and strength.
11. Stay Informed and Seek Early Intervention:
Educate yourself about the signs of TMJ issues. If you experience persistent jaw pain, clicking, or limited movement, seek early intervention from a healthcare professional.
By incorporating these prevention tips into your lifestyle, you can foster optimal jaw health and reduce the risk of TMJ disc dislocation. If you have specific concerns or experience symptoms, consult with Dr. Anurag Bhargava for personalized guidance.